By Crystal Chu
With an estimated total of 1.9 million new cases in 2022, cancer—the second most common cause of death in the USA—is projected to cause 609,360 nationwide deaths in 2022 [1]. Thus, identifying cancer in its early stages before tumors spread to multiple organs is imperative. However, this task is easier said than done: tumors are masters of stealth. Antibody-based therapeutic strategies are “beyond the reach” for oncogenic driver mutations, which pushes both the initiation and maintenance of cancer, as they are intracellular and thus limit the main detection process of targeting tumor cell surface antigens [2]. Although the covalent inhibitor sotorasib, an FDA approved medication, exists, it’s not effective for all patients. Thus, UCSF researchers (Ziyang Zhang, Peter J. Rohweder, Chayanid Ongpipattanakul, Koli Basu, Markus-Frederik Bohn, Eli J. Dugan, Veronica Steri, Byron Hann, Kevan M. Shokat, and Charles S. Craik) have investigated the use of the covalent inhibitor ARS1620, which harbors similarities to sotorasib, to bind and target the K-RAS (G12C) mutation. This bounded complex thus prompted researchers to create a new immunotherapy strategy to help detect and eliminate tumor cells with the help of T-cells: cancer treatment has taken a promising step forward.
T-cells have a very important, yet difficult job to accomplish. Dr. Zhang, one of the co-first authors of the original manuscript, explains in an interview the inner workings and role of the body’s T-cells through a dumpster diving analogy: “every single cell in our body has a [garbage disposal which] takes [unnecessary] proteins, [AKA “paper”] and shreds it…now we have settler proteins. Some of those pieces are brought out of the cell and spread all around. Now, we just think of dumpster diving as T-cells coming and looking at all the paper trash brought out of the cell and saying, ‘this cell looks suspicious [and this protein piece isn’t supposed to be here]…because there’s a virus inside. So I’m going to kill this virus-infected cell.’” Sorting through all the bits of shredded information, T-cells have the tedious task of spotting abnormalities. But, if the paper pieces were to be “highlighted,” this would significantly increase efficiency as T-cells would be able to easily pinpoint abnormalities. Thus, UCSF researchers created a cellular process to help assist the body’s T-cells. These irregular paper pieces are likened to K-RAS (G12C), a protein which, when malfunctioning, often drives oncogenic cancer mutations. This somatic mutation also allows the introduction of cysteine residue, which ultimately may be targeted by cell-permeable drugs and allow antibody recognition. The chemical inhibitor ARS1620 targets and reacts with the acquired cysteine residue, essentially binding to K-RAS (G12C) and “highlighting” the cancer protein. Then, when T-cells evaluate the many proteins projected outside of the cell, they can detect the haptenated peptide and kill the cell with an oncogenic mutation inside. Ultimately, it creates a peptide-MHC class I complex—a structure expressed on the surface of nucleated cells which displays peptide fragments that therapeutic antibodies can recognize and evaluate. To further support our T-cells, UCSF researchers created a bispecific antibody that essentially grabs the drug-labeled peptide and T-cell, effectively directing our T-cells toward the peptide.
UCSF researchers first investigated whether ARS1620-modified K-RAS (G12C) peptides are able to endure antigen presentation machinery and thus generate tumor-specific neoepitopes (peptides generated from somatic mutations and are seen as a target). Previously, it was unknown whether attaching an inhibitor, in this case ARS1620, would interfere with antigen processing and binding to MHC class I complexes. Thus, UCSF researchers hypothesized that K-RAS (G12C) could withstand the process of creating tumor-specific antigens that T-cells would recognize and target outside the cell’s surface. Focusing on two common MHC class I alleles, UCSF researchers synthesized two peptides, KK5-ARS and V7-ARS. These newly synthesized peptides were able to form MHC class I complexes with the alleles, suggesting that although modified by covalent inhibitors, the MHC class I complexes are secure and functional. Ultimately, these results confirm that K-RAS peptides can be bound by two common MHC class I alleles and that inhibitor modification of the peptide is tolerable.
The UCSF researchers’ next goal was to discover antibody fragments that specifically bind ARS1620-modified peptides by using a naive human B cell-derived Fab phage library in order to enable therapeutic targeting. Thus, they generated a gene that produces antibodies from human B cells, and then put that gene into the virus (phage) to create a phage library. With this, UCSF researchers were able to essentially isolate antibodies and discover which antibody fragments have the ability to bind to the ARS1620-modified complex. With five clones demonstrating a high-affinity binding to an ARS1620-labeled peptide, the P1A4 clone was selected based on its relatively short heavy-chain complementarity-determining region 3, along with selectivity for ARS1620. Simply put, UCSF researchers selected the P1A4 clone based on how tightly the antibodies bind to their target. As P1A4 was able to bind to the labeled complexes as opposed to unlabeled ones, the clone was suggested to have a select affinity for ARS1620-haptenated MHC class I complexes.
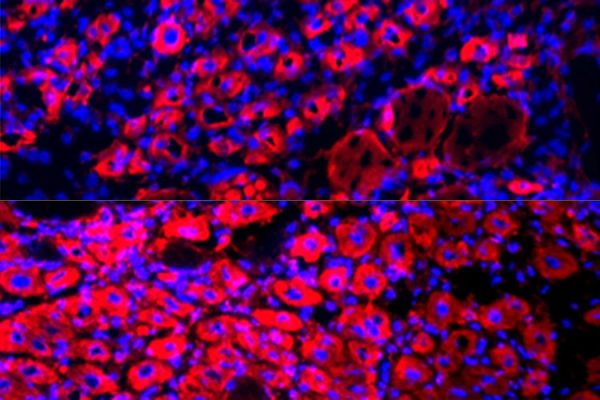
UCSF researchers then supported their claim that K-RAS (G12C) cells are able to present ARS1620-modified peptides in the MHC class I complex. With techniques such as immunoprecipitation—a technique using antibodies and agarose beads to target antibodies and isolate biomolecule-like proteins—and western blot—an approach involving gel electrophoresis and an antibody probe in order to analyze individual proteins—researchers concluded that treatment with ARS1620 was processed and presented in the MHC class I complex (the cell surface). Furthermore, this suggests that antigen-processing steps are able to tolerate the presence of ARS1620-labeled cysteine residues and confirm its overall existence.
Because not all K-RAS (G12C) mutant cells are responsive to direct chemical inhibition of K-RAS, there are clear limitations with this process. To compensate for these constraints and to support the claim that immunotargeting of a hapten adduct is a valid approach to overcome intrinsic drug resistance, UCSF researchers converted P1A4 into a BiTE (bispecific T-cell engager.) With a BiTE, T-cells and tumor cell antigens are bounded simultaneously, allowing the T-cell to be directed to the mutated ARS1620 labeled K-RAS peptide. This intrinsic resistance was overcome by the cellular conversion, allowing a proficient helper tool for T-cells detecting abnormalities. Another consideration would be that patients are resistant after receiving K-RAS (G12C) inhibitor treatment. The team wanted to investigate whether their approach would be effective against “clinically observed drug-resistant mutations” [2]. After experimenting on mice, it was reassured that K-RAS (G12C) mutation and appropriate MHC class I haplotypes are required for the presentation of ARS1620. Ultimately, this confirmed that given the proper chemical conditions, ARS1620-derived epitopes are detectable, and identification occurs.
Cancer affects a large portion of society, a large portion of oncogenic mutations being specifically driven by K-RAS (G12C). Although previous research has allowed our society to have readily available FDA-approved drugs, these drugs are not 100% effective as patient response varies. There are two populations of patients who may require additional help: those with appropriate mutations but have an unresponsive immune system and patients whose cancer outsmarts drugs by acquiring additional mutations to bypass the drug’s function. Dr. Zhang recognizes that the “work we’re talking about today can bring in another immunological component to [K-RAS (G12C) inhibitors] and bring our T-cells to target [and kill] these cancer cells even though the drug isn’t stopping cancer…[this would help] benefit those two populations.” This promising new immunotherapy strategy would help save patients’ lives and spark new interest within the science community for related research.
With an influx of various factors compiled into one goal, conducting research is a continuous and tedious process. Despite the trial-and-error associated with the scientific process, Dr. Zhang advocates that it’s imperative to “enter each day with a positive mindset,” and that he’s “excited to discover better antibodies to help kill tumors and bring in a new strategy to treat cancer.” Even though the UCSF team is still showing their proof of concept in culture for cancer cells, Zhang predicts that “once [they] have a proof of concept, [they] can start to move toward therapeutic applications.” The future of immunotherapy is promising and contributing toward a healthier society.
[1] ACS Medical Content and News Staff. “2022 Cancer Facts & Figures Cancer: Cancer Death Rate Drops.” American Cancer Society, American Cancer Society, 12 Jan. 2022, https://www.cancer.org/latest-news/facts-and-figures-2022.html.
[2] Ziyang Zhang, Peter J. Rohweder, Chayanid Ongpipattanakul, Koli Basu, Markus-Frederik Bohn, Eli J. Dugan, Veronica Steri, Byron Hann, Kevan M. Shokat, and Charles S. Craik. “A covalent inhibitor of K-Ras(G12C) induces MHC class I presentation of haptenated peptide neoepitopes targetable by immunotherapy.” Cancer Cell, Elsevier Inc, 4 Aug. 20222,DOI: https://doi.org/10.1016/j.ccell.2022.07.005