by: Vimathi Gummalla
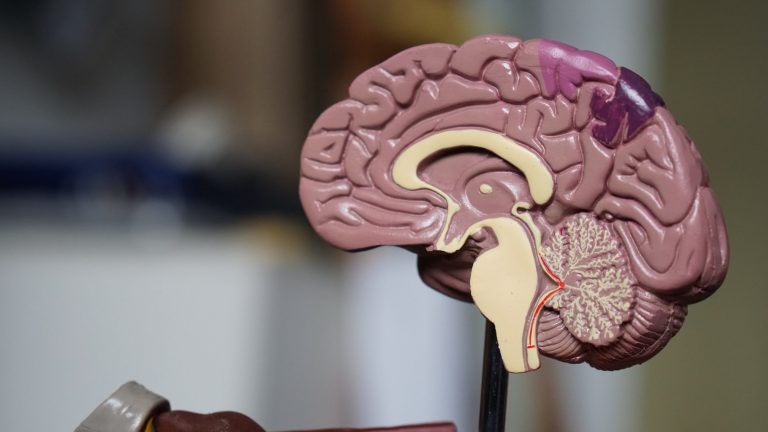
Immunotherapy is a rising field in which treatment boosts the body’s own natural defenses to fight diseases like cancer. However, one specific area that continues to complicate the innovative treatment is the brain. To simplify the problem, scientists created T-cell therapy, where scientists genetically alter a patient’s T-cells to work in a certain way. Earlier this year, the Okada Lab at the University of California San Francisco studied the success of these genetically engineered T-cells. Their goal was to describe immunotherapy in a brain tumor setting. As Postdoctoral Scholar Dr. Polly Chuntova explains, “our ability to engineer and manipulate such a small object, as T-cells are even smaller than normal cells, is truly amazing.” Their findings not only illustrate a number of key challenges, but also demonstrate a promising approach to a personalized and less infiltrative treatment, especially in the brain.
In the context of this study, the lab focused on glioblastoma (GBM), a highly aggressive and invasive tumor that originates in the brain but spreads to other parts of the body. GBM develops through a series of progressions that eventually builds up to highly violent cancer. With an average survival rate of only fifteen months following diagnosis, GBM is one of the most common aggressive tumors. Once diagnosed, patients often undergo tumor resection in which the maximum amount of tissue that is safe to cut out is directly removed from the tumor site; treatment is continued with radiotherapy and chemotherapy. Although these treatments generally show positive results in reducing tumor growth, they carry many dangerous side-effects because the radiation and chemicals from the treatment spread to healthier parts of the body. Additionally, GBM responds poorly to both treatments, so there remains a high likelihood of recurrence. For these reasons, scientists agree that finding an approach that hones the treatment to the tumors’ site is necessary and urgent.
Thus came about the field of immunotherapy. In general, immunotherapy includes techniques ranging from vaccines to human-made antibodies to altered T-cells. In each, there exists a limited hands-on and personalized procedure. The main purpose is to directly insert an altered protein or cell and let the patient’s own immune system adapt to it. This way, an overflow of chemicals or radiation found in past treatments is minimized. In treating most cancers, genetically altered T-cells is the best method of immunotherapy. Specifically, this study utilizes chimeric antigen receptor (CAR) T-cell therapy to treat GBM. It is a type of immunotherapeutic procedure in which doctors’ collect and use the patient’s T-cells to treat their cancer. Naturally, the role of T-cells is to destroy any detected infected cells; genetically engineered T-cells harness the same power, but they target only the tumor. The procedure is as follows: collection and isolation of the T-cells from a sample of the patient’s blood, genetic modification of the cells to produce specific CAR receptors on their surface, and the infusion of the new CAR T-cells in the bloodstream. The receptors can now easily recognize the target, kill the tumor cells, and ideally destroy the cancer.
Though the general cure is outlined, immunotherapy for GBM has its own set of challenges. First and foremost, the brain is a part of the body like no other. It is a highly sensitive organ in which any procedure that damages its tissue could have serious and irreversible consequences. In this research, the key challenges include the blood-brain barrier, immunosuppression at the tumor site, and antigen heterogeneity. Firstly, the blood-brain barrier (BBB) is a semi-permeable border around the brain that prevents bacteria and toxins in the blood from entering. In doing so, the BBB also blocks out lymphocytes that could potentially kill the tumor. Interestingly, the BBB is still intact in areas where the cancer cells infiltrate the normal brain tissue, so it is possible for cells to pass through. The challenge is to ensure that the CAR T-cells are a part of those selected cells and can actually reach the tumor site within the brain. Second, tumors often use a process known as immunosuppression, where the tumor builds a microenvironment that enables the growth of cancer cells while halting that of T-cells. The engineering of the T-cells must be careful as to avoid getting shut down by this environment.
Lastly, due to antigen heterogeneity, antigens are too diverse for scientists to know which one is best to bind to. Antigens are foreign substances, in this case signals from tumor cells, that trigger the immune system to produce antibodies that then recognize and kill the cell on which the antigens are on. Tracking antigens is important because each is like an identification tag for a drug or mechanism to easily target. The key challenge in this study and the technology it uses is finding the right antigen that lies only on tumor cells. If the antigen is not specific to cancer cells, then the T-cells might also attack healthy cells. Therefore, the current goal is to explore the availability of such antigens and their success with the genetically engineered T-cells. As Kira M. Downey, a junior specialist at the Okada lab, shared, “the most exciting part of CAR T-cell technology is that we are now trying to hit more than one targets,” to then come up with a kind of combination of antigens that is tumor-specific.
Due to limited evidence of CAR T-cell therapy, the paper discussed four different trials, but two in particular showed significant results. In one, scientists treated 10 GBM patients who had EGFRvIII-specific CAR T-cells infused through their veins. EGFRvIII is an epidermal growth factor receptor previously found to be over-expressed in GBM patients, but not in normal tissue. The same mutation was researched to enhance resistance to both chemotherapy and radiotherapy. Throughout the trial, the team collected data and saw counteractive results in only one patient; also, none of the patients suffered off-tumor toxicities, which is when the cells start to attack healthy cells expressing the same target antigen. This meant that the CAR T-cells successfully entered the bloodstream, passed through the BBB, and reached the tumor site, which overall, decreased the expression of EGFRvIII in tumor cells.
In another trial, the epidermal growth factor receptor called HER2 was targeted. This trial was done on 17 GBM patients, and 8 of them responded positively; 7 had stable diseases and 1 faced some side-effects. Unfortunately, the CAR T-cells did not infiltrate the barrier and remained only on the outer rim of the tumor site. Because of this, the need to develop new methods still exists. Even though all four clinical trials demonstrated positive profiles, the data further emphasized the continued challenges among successful CAR T-cell therapy for GBM.
Working to develop an effective immunotherapy treatment is a very long and complex process. Postdoctoral Scholar Dr. Bindu Hedge says that “when moving forward, they have to consider the different aspects at once and tackle the challenges all together.” But, with more challenges comes a greater motivation to innovate and invent new technologies, and the future of immunotherapy for GBM is full of more creative and advanced solutions.